Explainer: data shows maternal death takes a downwards trend
In recent weeks, the mainstream and social media have been saturated with news on maternal death at the various health facilities in The Gambia.
The news generated fear, apprehension and concern from the public, leading to a number of protests, both online and on the streets. It also triggered debates about the risk associated with childbirth at public health facilities.
Dr Musa Marena, a gynecologist, is the head of the health ministry’s unit responsible for maternal health.
“We are receiving reports that some people are avoiding the [public] health centers and hospitals because of fear that it is not safe to deliver in these places,” said Dr Marena.
“And when complications arise because of the time they take hesitating to visit the health facilities, it is often late to [save] some of them.”
This factsheet contains the trend of maternal death in the country as well as the major causes, and what is being done about it.
The stats show decline in maternal death
There is very little availability of adequate and reliable data that deals with emergency obstetric care in The Gambia from open sources. But, there are some studies on the issue, including performance audit published by the National Audit Office (NAO) in September 2020.
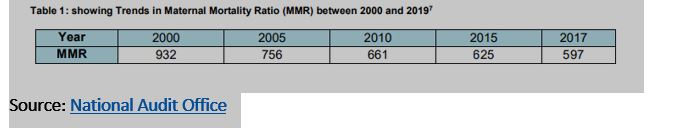
According to the NAO study, over the years, The Gambia has made significant progress in reducing maternal mortality rate. However, the country is far behind in meeting the Sustainable Development Goal target of reducing maternal mortality ratio (MMR) to less than 70 per 100,000 live births by 2030.
The Gambia’s overall reduction rate in MMR between the year 2000 and 2017 is 36.8%.
All the data collected from various sources shows a decline in maternal death. But there are variances. For example, the results from the Demographic Health Survey 2019/2020 estimated that the MMR, in the 7 years preceding the survey, was at 289 maternal deaths in every 100,000 live births. And pregnancy related death within the same period was 320 for every 100,000 live birth.
“… for every 1,000 births in The Gambia, about 3 women die during pregnancy or within 2 months of the end of a pregnancy from any cause including accidents or violence,” states the demographic health survey.
A more recent data on MMR has been published by the Ministry of Health in the first week of October for years 2019 and 2020. The data gathered from public health facilities across the country showed that MMR has declined from 221 deaths per 100, 000 live births in 2019 to 169 deaths per 100,000 live births.
There is a significant regional variance in the MMR. While Central River Region witnessed a decline from 2019 to 2020, the North Bank Region witnessed an increase. For example, North Bank recorded 388 MMR per 100, 000 live births in 2020 compared to 82 per 100, 000 in 2019. Whereas the Central River Region witnessed a decline from 349 per 100, 000 live births in 2019 to 152 per 100, 000 in 2020.
Causes of maternal death
Though the data shows a decline in maternal deaths, the figures are still unacceptably high, said the NAO in their performance audit.
“For The Gambia to achieve the target of having less than 140 deaths per 100,000 live births in MMR by 2030 (SDG 3), it needs to achieve an overall reduction rate of 77% from the 2017 figure, more than twice the current reduction rate,” said the NAO.
According to data recorded by the Reproductive, Maternal, Neonatal, Child and Adolescent Health Department of the health ministry, maternal deaths are largely due to “avoidable” complications such as hemorrhage (37%), hypertensive disorders of pregnancy (11%) and sepsis (11%).
Causes of complications
The data from the Health Ministry shows at least 15% of all pregnant women will develop complications during pregnancy, labour or postpartum.
Dr Marena said some of the complications cannot be prevented or even predicted. Education, nutrition and childhood immunization, male involvement, financial and social empowerment of women, family planning will help prevent some of these complications, he said.
Other issues responsible for complications during childbirth include teenage pregnancy, anaemia, short interpregnancy intervals, poor nutrition, pregnancy whilst being sick and pregnancy at old age.
“Prenatal and antenatal care as well as birth preparedness will help with early detection and management of some of these complications,” said Dr Marena.
“Birth preparedness and complication readiness will prevent the delay in recognizing danger signs, in decision making or delay in reaching the health facility.”
Limited, ill-equipped EmOC
As part of their performance audit of emergency obstetric care across the country, the NAO observed the following weaknesses in the health care delivery.
n Most of the facilities have the capacity to provide basic emergency obstetric care (EmOC) functions. However, there are equipment and human capacity gaps in the provision of assisted vaginal delivery to complete the set of basic EmOC functions.
n There are gaps in the provision of comprehensive EmOC services as more than half of the mandated CEmOC centres are not providing either blood transfusion or both blood transfusion and caesarean section, also known as C-section.
The Lower River Region has no CEmOC centre, delaying access to comprehensive EmOC for women in that region.


